Strategies, Tools, and Self-Empowerment for Handling Migraine In Case Book Work
Understanding Diagnosis through Casebook Work
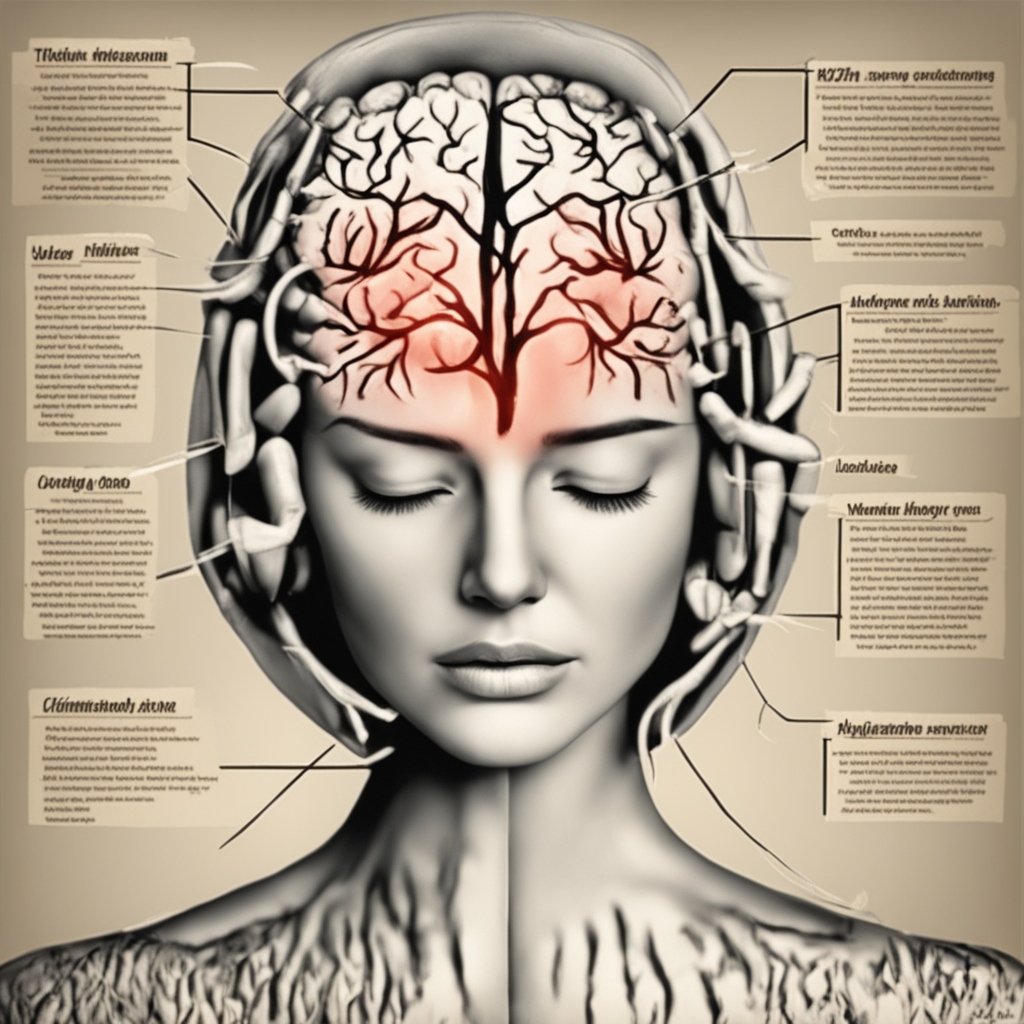
A migraine’s signs and symptoms are used to make the diagnosis. Although neuroimaging studies are not required to diagnose migraine, they can be utilized to identify other headache causes in patients whose physical examination and medical history do not support a diagnosis of migraine. It is thought that a sizable portion of those who have the illness go undetected.
The International Headache Society states that the “5, 4, 3, 2, 1 criteria,” which are as follows, can be used to diagnose migraine without aura:
- Five or more attacks—two attacks are enough to diagnose a migraine with aura.
- Length: four hours to three days
- At least two of the subsequent:
Unilateral (affecting just one head side)
Stuttering
The degree of moderate to severe pain
Made worse by or contributing to an avoidance of regular exercise
- At least one of the subsequent:
Feeling sick or throwing up
Light and sound sensitivity (photophobia and phonophobia)
The diagnosis is more likely if a patient has two of the following symptoms: photophobia, nausea, or a daytime inability to work or study. The likelihood that this is a migraine attack is 92% in those who have four out of five of the following symptoms: pulsing headache, duration of 4–72 hours, headache pain on one side, nausea, or symptoms that interfere with daily life. The likelihood is 17% for people who have fewer than three of these symptoms.
Classification In 1988, migraines were first categorized thoroughly
In 2004, the International Headache Society revised their classification system for headaches. In 2018, a third edition was released. This classification includes headaches of the tension variety, cluster headaches, and migraine as primary headache disorders.
There are six subclasses of migraine (some with additional subclasses within them):
- The term “common migraine” refers to migraine headaches that do not have an aura.
- The term “classic migraine” refers to migraines that typically include aura in addition to migraine symptoms. Aura can less frequently happen with or without a headache (i.e., nonmigraine headache). There are two distinct types of migraine: familial hemiplegic migraine and sporadic hemiplegic migraine. In the former case, the patient experiences aura-accompanied motor weakness. “Familial” refers to the condition if a close relative has had it; “sporadic” refers to less frequent occurrences.Another type of migraine is called basilar-type, in which there is no motor weakness but rather trouble speaking, dizziness, ringing in the ears, and other brainstem-related symptoms in addition to a headache and aura.
- At first, it was thought that this kind resulted from spasms in the basilar artery, which nourishes the brainstem. The appropriate term for this clinical condition is migraine with brainstem aura (MBA), as it is no longer thought to represent the fundamental etiology. In contrast to visual or optical migraine, retinal migraine is characterized by migraine headaches along with visual abnormalities or even transient blindness in one eye.
- Childhood periodic syndromes, such as benign paroxysmal vertigo of childhood (occasional attacks of vertigo), abdominal migraine (abdominal pain, generally accompanied by nausea), and cyclical vomiting (occasional strong periods of vomiting) are frequently antecedents to migraine.
Migraine in the Abdomen

There is debate over the diagnosis of abdominal migraine. There is evidence to suggest that recurrent bouts of stomach discomfort without accompanying headaches could be a form of migraine or at least a sign of one.
These pain bouts usually last from minutes to hours and may or may not be preceded by a prodrome similar to that of a migraine.
People who have a personal or family history of typical migraine are more likely to experience them. Other illnesses including infantile benign paroxysmal vertigo and cyclical vomiting syndrome are thought to be antecedents.
Differential Diagnosis
 Acute glaucoma, subarachnoid hemorrhage, meningitis, temporal arteritis, cluster headaches, and migraines are among other illnesses that might resemble a migraine in their symptoms. Meningitis with fevers, subarachnoid hemorrhage with a very quick onset, acute glaucoma with vision problems, and cluster headaches with one-sided nose stuffiness, tears, and excruciating pain around the orbits are the typical symptoms of temporal arteritis, which usually affects people over 50.
Acute glaucoma, subarachnoid hemorrhage, meningitis, temporal arteritis, cluster headaches, and migraines are among other illnesses that might resemble a migraine in their symptoms. Meningitis with fevers, subarachnoid hemorrhage with a very quick onset, acute glaucoma with vision problems, and cluster headaches with one-sided nose stuffiness, tears, and excruciating pain around the orbits are the typical symptoms of temporal arteritis, which usually affects people over 50.
Tension headaches are less incapacitating, usually don’t pound, and usually affect both sides.
Neuroimaging to rule out other intracranial diseases should not be performed on patients with consistent headaches that fit the criteria for migraines.
This necessitates the absence of additional alarming symptoms such papilledema, or enlargement of the optic disc.
There is no greater chance for people who have migraines to experience severe headaches from another source.
Let’s discuss Prevention in Casebook Work
Medication, dietary supplements, lifestyle modifications, and surgery are among the preventive therapies for migraines. For persons who get headaches more than twice a week, are intolerant of the drugs used to treat acute attacks, or have severe episodes that are difficult to control, prevention is advised. Cessation of tobacco usage and reduction of sleep-inducing behaviors are recommended lifestyle adjustments.
Reducing the incidence, severity, and length of migraine attacks while improving the efficacy of abortive medication are the objectives. Preventing drug overuse headaches is another reason to practice prevention. This is a frequent issue that may cause a persistent headache every day.
Drugs
 If a preventive migraine medicine lowers the frequency or intensity of migraine attacks by 50% or more, it is deemed beneficial. Many medications, including beta-blockers, anticonvulsive agents like topiramate or sodium valproate, antidepressants like amitriptyline, and calcium channel blockers like flunarizine, are used off label for the preventative treatment of migraine headaches because there aren’t many that are approved specifically for this purpose.
If a preventive migraine medicine lowers the frequency or intensity of migraine attacks by 50% or more, it is deemed beneficial. Many medications, including beta-blockers, anticonvulsive agents like topiramate or sodium valproate, antidepressants like amitriptyline, and calcium channel blockers like flunarizine, are used off label for the preventative treatment of migraine headaches because there aren’t many that are approved specifically for this purpose.
The anticonvulsants topiramate and divalproex/sodium valproate, as well as the beta blockers propranolol and metoprolol, are rated by guidelines as having the highest level of evidence for first-line usage in the prevention of migraines in adults. This rating is pretty consistent. The strongest data is found in children with propranolol plus topiramate; nevertheless, as of 2020, the data only shows short-term benefit.
Timolol, a beta blocker, is also useful in preventing migraines and lessening the frequency and intensity of migraine attacks. Although beta blockers are frequently employed as first-line therapy, verapamil, a calcium channel blocker, and candesartan, an angiotensin receptor blocker, are two other antihypertensives that have been shown to be effective in preventing migraines.
Anti-calcitonin gene-related peptide-containing medications, such as eptinezumab, erenumab, galcanezumab, and fremanezumab, seem to reduce migraine incidence by one to two episodes per month.
Alternative Medical Interventions
 Compared to sham acupuncture, which uses needles that are inserted haphazardly or do not enter the skin, acupuncture has a negligible effect on the frequency of migraine attacks. Although the research had significant methodological issues, physiotherapy, massage, relaxation techniques, and chiropractic manipulation may be just as beneficial as propranolol or topiramate in preventing migraine headaches. However, a different evaluation discovered that the evidence for spinal manipulation was weak and not strong enough to justify its application.
Compared to sham acupuncture, which uses needles that are inserted haphazardly or do not enter the skin, acupuncture has a negligible effect on the frequency of migraine attacks. Although the research had significant methodological issues, physiotherapy, massage, relaxation techniques, and chiropractic manipulation may be just as beneficial as propranolol or topiramate in preventing migraine headaches. However, a different evaluation discovered that the evidence for spinal manipulation was weak and not strong enough to justify its application.
The use of stress-reduction strategies like biofeedback, cognitive behavioral therapy, and relaxation techniques is supported by some preliminary data. Frequency may reduce with regular activity. Many psychological strategies, such as educational approaches, relaxation techniques, help in developing coping mechanisms, strategies to alter one’s perception of a migraine attack, and strategies to lessen symptoms, have been developed with the goal of preventing or decreasing the frequency of migraine in adults. Additional tactics consist of behavioral training, biofeedback, acceptance and commitment therapy, progressive muscle relaxation, and mindfulness-based therapies. There is a dearth of medical evidence to support the efficacy of these psychological methods.
Melatonin as an adjunctive therapy for migraine prevention and treatment appears to have some support. Data on melatonin are conflicting, and some research has produced unfavorable findings. Although the exact causes of the contradictory results are unknown, variations in study design and dose may be to blame. Although the exact mechanisms of action of melatonin in migraines are unknown, they could involve better sleep, direct impact on melatonin receptors in the brain, and anti-inflammatory qualities.
Instruments and Operations
 Medical devices like neurostimulators and biofeedback have some benefits in preventing migraines, primarily when overusing drugs or when standard anti-migraine medications are contraindicated. In order to manage various physiological characteristics and attempt to relax, people can benefit from biofeedback. It may also be an effective way to cure migraines.
Medical devices like neurostimulators and biofeedback have some benefits in preventing migraines, primarily when overusing drugs or when standard anti-migraine medications are contraindicated. In order to manage various physiological characteristics and attempt to relax, people can benefit from biofeedback. It may also be an effective way to cure migraines.
Intractable chronic migraines can be treated with neurostimulation, which uses noninvasive or implantable neurostimulators that resemble pacemakers. For severe instances, the outcomes are positive.
In the US, migraine prophylaxis is permitted with the use of both transcranial magnetic stimulation and transcutaneous electrical nerve stimulation.Additionally, there is a possibility that transcutaneous electrical nerve stimulation reduces the frequency of migraine attacks.
For some patients who do not respond to medication, migraine surgery, which includes decompressing specific nerves around the head and neck, may be a possibility.
How can manage the casebook work in the migraine guide?
Treatment consists of three primary components: medicine for prevention, acute symptomatic control, and trigger avoidance. Early in an attack, medication has a greater impact. A condition known as medication overuse headache, in which headaches worsen and occur more frequently, can be brought on by taking drugs frequently.
Ergotamines, triptans, and analgesics—particularly opioid analgesics—may cause this. It is advised not to use basic analgesics more than three days a week at most because of these worries.
Ibuprofen reduces pain in children and is the first prescribed medication. It doesn’t seem like paracetamol works well for relieving pain. Although there is a chance of mild side effects such taste disruption, nose problems, dizziness, exhaustion, poor energy, nausea, or vomiting, triptans are effective. To reduce the risk of drug overuse headache, ibuprofen should be taken less than half of the days in a month and triptans less than a third.
Painkillers
 Simple analgesics like nonsteroidal anti-inflammatory drugs (NSAIDs) or a combination of paracetamol (also known as acetaminophen), aspirin, and caffeine are recommended as the first line of treatment for individuals with mild to moderate symptoms.
Simple analgesics like nonsteroidal anti-inflammatory drugs (NSAIDs) or a combination of paracetamol (also known as acetaminophen), aspirin, and caffeine are recommended as the first line of treatment for individuals with mild to moderate symptoms.
However, excessive caffeine consumption can both contribute to and trigger migraine chronification in many patients. There is evidence to support the usage of certain NSAIDs, such as ibuprofen and diclofenac.
Aspirin (900–1000 mg) works similarly to sumatriptan to alleviate moderate–to severe migraine discomfort. There are intramuscular and intravenous versions of ketorolac available.
Another efficient medication with a little chance of side effects is paracetamol, either used alone or in conjunction with metoclopramide. Intravenous metoclopramide works well on its own as well. Metoclopramide, paracetamol, and other NSAIDs are considered safe during pregnancy up until the third trimester.
Since naproxen is only marginally more effective than a placebo in clinical trials, it may not be a suitable treatment for migraines on its own.
Triptans
 Sumatriptan is one of the triptans (an abortive medicine) used to treat an active migraine headache. When someone has moderate to severe pain from an acute migraine headache, or when their symptoms are milder but they don’t go away with basic analgesics, triptans are the first recommended course of treatment. Up to 75% of patients have indicated that triptans are beneficial for treating both pain and nausea. Sumatriptan can be administered by oral (by mouth), injection (subcutaneous), rectal, nasal spray, or oral dissolving pills, among other ways.
Sumatriptan is one of the triptans (an abortive medicine) used to treat an active migraine headache. When someone has moderate to severe pain from an acute migraine headache, or when their symptoms are milder but they don’t go away with basic analgesics, triptans are the first recommended course of treatment. Up to 75% of patients have indicated that triptans are beneficial for treating both pain and nausea. Sumatriptan can be administered by oral (by mouth), injection (subcutaneous), rectal, nasal spray, or oral dissolving pills, among other ways.
It may be challenging to take the preventive medication by mouth or through the nose for those who experience nausea or vomiting as a result of a migraine. The effectiveness of all delivery routes in relieving migraine symptoms has been demonstrated; however, nasal and injectable subcutaneous injection may cause higher adverse effects. The side effects linked to rectal administration have not been thoroughly investigated. It’s possible for some people to react more favorably to one kind of sumatriptan than another.
Sumatriptan has no effect on the onset of subsequent migraine attacks. Combining sumatriptan with naproxen may be recommended as a combination therapy to boost effectiveness in reducing migraine symptoms.
Antagonists of GRP receptors
In order to prevent or lessen the severity of migraine headaches, calcitonin gene-related peptide or its receptor is the aim of calcitonin gene-related peptide receptor antagonists (CGRP). A powerful vasodilator and signaling molecule, CGRP plays a role in the onset of migraine headaches. In phase III randomized clinical studies, the four injectable monoclonal antibodies that target CGRP or its receptor—eptinezumab, erenumab, fremanezumab, and galcanezumab—have shown promise in the prophylactic treatment of episodic and chronic migraine headaches.
In March 2023, zavegepant received FDA approval for medicinal use in the US.
Ergotamine-containing substances
Older drugs that are still prescribed for migraines are ergotamine and dihydroergotamine; the latter is available as an injectable and nasal spray. They have side effects that are usually mild and seem to be just as effective as triptans. They seem to be the best course of action in the most severe instances, such as those involving status migrainosus. They should not be used in patients who have coronary artery disease because they can induce vasospasm, particularly coronary vasospasm.
Magnesium
It is well known that magnesium is a cheap, over-the-counter supplement that can be used in conjunction with other treatments to reduce migraines. has been demonstrated in certain studies to be useful in the intravenous treatment and prevention of migraine. Oral magnesium reduces migraine frequency and intensity; the intravenous form reduces attacks as measured in around 15–45 minutes, 120 minutes, and 24-hour time periods.
The Migraine History
Written in ancient Egypt circa 1500 BCE, the Ebers Papyrus has an early account that is compatible with migraine. Writings from the Hippocratic school of medicine date back to 200 BCE, and they spoke about a visual aura that could appear before a headache and how vomiting could provide some relief.
Aretaeus of Cappadocia classified headaches into three categories in the second century: cephalalgia, cephalea, and heterocrania. The term “half-head,” or “hemicrania,” was used by Galen of Pergamon and is ultimately where the word “migraine” originated. Additionally, he suggested that the headache’s blood vessels and meninges were the source of the discomfort. French librarian Louis Hyacinthe Thomas initially classified migraines into the two currently recognized forms in 1887: migraine with aura (migraine ophthalmique) and migraine without aura (migraine vulgaire). The visual aura seen during a migraine is congruent with Hildegard von Bingen’s spiritual visions, which she referred to as “reflections of the living light”.
Trepanation dates back to 7,000 BCE, when holes were purposefully drilled into a cranium. Although some people have survived the surgery, many would have perished from infection. “Letting evil spirits escape” was said to be how it worked. In the seventeenth century, William Harvey suggested trepanation as a remedy for migraines. The historical correlation between trepanation and headaches might well be a myth or idle conjecture that developed years later. Famous American physician William Osler misconstrued the remarks made by French anthropologist and physician Paul Broca in 1913 regarding a collection of Neolithic kid skulls he had discovered in the 1870s. There were no visible symptoms of fractures on these skulls that would have justified this intricate surgery for purely medical purposes.
Trepanation most likely originated from superstitions to exorcise “confined demons” from the head or to make lucky or healing talismans from the broken bones in the patients’ skulls. But in an effort to make Broca’s idea more acceptable to his contemporary audiences, Osler clarified that trepanation treatments were only used to minor ailments like “infantile convulsions headache and various cerebral diseases believed to be caused by confined demons.”
Although numerous migraine remedies have been tried, the usage of a medication that later proved to be beneficial did not begin until 1868. This material was the ergot fungus, which 1918 saw the isolation of ergotamine. The first triptan, sumatriptan, was created in 1988, and methylsergide in 1959. In the 20th century, effective preventive strategies were discovered and validated thanks to improved study designs.
Conclusion | Casebook Work-Based Migraine Guide
On sum up, this guide on migraines, painstakingly created through casebook work, provides an invaluable tool for people suffering from this crippling ailment.
Through examining actual situations and combining professional opinions, it sheds light on the way to comprehend, control, and eventually overcome migraine.
Equipped with an understanding of diagnosis, prevention, and management techniques, readers can set out on a path to increased autonomy and enhanced quality of life.
We can work toward a time when millions of people’s lives are free from migraine headaches by furthering research, raising awareness, and fostering patient-professional partnership.
image courtesy
Mikhail Nilov, MART PRODUCTION, Alex Green ,Anna Shvets, Pixabay, Alex Green, Mahdi Bafande.
